What Causes Cyst Formation In Polycystic Kidney Disease?

What is polycystic kidney disease?
Polycystic kidney disease (PKD) is a prevalent genetic disorder, impacting approximately 500,000 individuals in the United States. The autosomal dominant form of the disease is significantly more widespread than the autosomal recessive form. Autosomal dominant polycystic kidney disease affects approximately 1 in 500 to 1,000 people, whereas the autosomal recessive type is estimated to occur in 1 in 20,000 to 40,000 individuals.
PKD causes many fluid-filled cysts to grow in the kidneys. Unlike the usually harmless simple kidney cysts that can form in the kidneys later in life, PKD cysts can change the shape of the kidneys, making them much larger than they should be and taking the place of normal kidney tissue. With less normal kidney tissue, the kidneys cannot function as well, and eventually, the kidneys may fail.
PKD can also cause other complications or problems, such as high blood pressure, cysts in the liver, and problems with blood vessels in the brain and heart.
Signs and symptoms of PKD
ADPKD doesn’t generally cause any signs or symptoms until the cysts are a half inch or larger.
Signs and symptoms include:
- Hypertension (high blood pressure)
- Pain in your back and side
- Blood in the urine
- Urinary tract infections
- Kidney stones
- Enlarged and painful abdomen
- Abnormal heart valves

Complications of PKD
While the kidneys are the organs that are primarily affected by PKD, it can also affect other parts of the body. Some of the complications of PKD may include:
- High blood pressure
- Urinary tract infections
- Kidney stones
- Liver cysts
- Cysts in your pancreas
- Heart valve problems
- Colon problems
- Brain aneurysms
- Diverticular disease
https://www.researchgate.net/publication/49806892_TRPP_channels_and_polycystins
The Pathology of Cyst Formation in PKD
This gets a little scientific but is excellent if you want to understand why, in my next post, I recommend using specific diets and herbs to treat and manage PKD. It will also give you a sound scientific understanding of the mechanism of cyst formation in the PKD model.
Cilia and their role in PKD
Cilia are tiny structures found in kidney cells that act as sensors. They can detect fluid flow and its composition and help regulate calcium movement in the cells. However, there is still some debate about how exactly cilia sense mechanical stimuli and control calcium signalling.
The cilia structure includes several parts: the axoneme, ciliary membrane, ciliary plasma, basal body, and transition zone. The ciliary membrane contains many receptors, ion channels, and sensory proteins, while the cilioplasm contains signalling and transport proteins. The axoneme and basal body are connected by a barrier called the transition zone, which separates the ciliary matrix from the cytoplasm. Problems with the structure and function of cilia can cause various diseases known as ciliopathies, including polycystic kidney disease (PKD).
In a healthy kidney, the length of renal cilia should be within a specific range. Changes in cilia length or their loss can lead to kidney problems. The assembly, disassembly, and cilia maintenance rely on intraflagellar transport (IFT). Mutations in IFT genes can contribute to PKD.

https://www.frontiersin.org/articles/10.3389/fphys.2021.693130/full
Glucose Metabolism and PKD
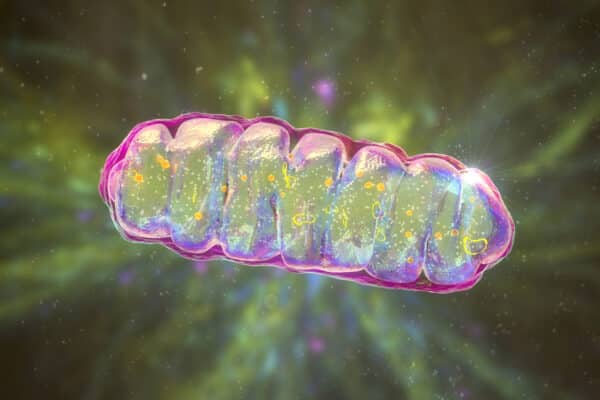
In normal cells, glucose is converted into a molecule called pyruvate through a process called glycolysis. Pyruvate is then used in the mitochondria, the cell’s energy powerhouse, to produce energy through a series of chemical reactions known as the tricarboxylic acid (TCA) cycle. This energy production process, called oxidative phosphorylation (OXPHOS), requires specific molecules like NADH and succinate.
However, in cells affected by cystic diseases, such as polycystic kidney disease (PKD), there is a change in how glucose is processed. Instead of going through the normal energy production pathway, pyruvate is converted into another molecule called lactate. This change in glucose metabolism is known as the “Warburg effect” or aerobic glycolysis. Similar metabolic changes have been observed in various studies using mouse and rat models and human samples of PKD.
Researchers have found that a compound called 2-deoxy-D-glucose (2-DG), similar to glucose but cannot be used for energy production, can reduce cyst growth in PKD animal models. Increased glycolysis in PKD leads to the accumulating of certain molecules called glycosphingolipids (GSLs). These GSLs can affect the function of cellular structures called cilia (mentioned above) and also lead to the release of harmful substances called reactive oxygen species (ROS), causing oxidative stress.
https://www.frontiersin.org/articles/10.3389/fphys.2021.693130/full
The mTOR Pathway
The mammalian target of the rapamycin (mTOR) pathway is a crucial regulatory pathway involved in cell growth, proliferation, and metabolism. It plays a significant role in the pathogenesis of several diseases, including Polycystic Kidney Disease (PKD).
Studies have demonstrated that the mTOR pathway is dysregulated in PKD. Increased mTOR activity has been observed in both ADPKD and ARPKD, contributing to cystogenesis.
The mTOR pathway integrates various signals, including growth factors, nutrients, energy status, and cellular stress, to regulate cell growth and proliferation. Dysregulation of this pathway leads to uncontrolled cell proliferation, fluid secretion, and cyst enlargement in PKD.
One of the major signalling complexes involved in mTOR pathway regulation is the mechanistic target of rapamycin complex 1 (mTORC1). mTORC1 activation promotes protein synthesis, cell growth, and metabolism. In PKD, mTORC1 activity is upregulated, leading to aberrant cell proliferation and cyst formation. The increased mTORC1 signalling contributes
to the expansion of cysts by promoting cell proliferation and inhibiting apoptosis (programmed cell death).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1459339/
The primary signalling inputs that activate mTORC1 in PKD include growth factors such as insulin and insulin-like growth factor 1 (IGF-1), which bind to their receptors and activate downstream signalling pathways like phosphoinositide 3-kinase (PI3K)/Akt. This activation results in the phosphorylation and inhibition of tuberous sclerosis complex 1/2 (TSC1/2), a negative regulator of mTORC1. Loss of TSC1/2 function in PKD leads to sustained mTORC1 activity, promoting cyst growth.
The dysregulation of mTORC1 also affects various cellular processes involved in cystogenesis. It promotes cell cycle progression, cell proliferation, and survival, increasing cell numbers within the cysts. Moreover, mTORC1 activation alters the balance between cell proliferation and apoptosis, favouring cell survival and preventing normal programmed cell death.
Targeting the mTOR pathway has emerged as a potential therapeutic strategy for PKD. Rapamycin and its analogs, known as mTOR inhibitors, have shown promise in preclinical studies and early-phase clinical trials for slowing cyst growth and preserving renal function in PKD patients. These inhibitors suppress mTORC1 signalling, thereby reducing cell proliferation and promoting apoptosis within the cysts.
https://www.sciencedirect.com/science/article/abs/pii/S1471491411001043

Cyclic AMP pathway
The Cyclic AMP pathway plays a crucial role in the growth of kidney cysts in autosomal dominant polycystic kidney disease (ADPKD).
The cyclic adenosine monophosphate (cAMP) pathway is a crucial intracellular signalling pathway that regulates various physiological processes in cells. It involves the activation of cell surface receptors, typically G protein-coupled receptors (GPCRs), which initiate a cascade of events leading to the production of cAMP and subsequent activation of downstream signalling pathways.
What causes elevated cAMP levels?
One reason is that there is an increase in a molecule called vasopressin receptor (V2R) in PKD, which stimulates the production of cAMP. By blocking V2R, researchers have been able to lower cAMP levels and slow down cyst development in mouse models and clinical trials.
Another possibility is that certain enzymes regulated by calcium, called adenylate cyclases (ACs) and phosphodiesterases (PDEs), may contribute to increased cAMP production. Studies have shown that certain ACs are overexpressed in PKD cells and that blocking them specifically in the cyst cells can reduce cyst growth. Similarly, specific PDEs play a role in regulating cAMP levels and cell proliferation in PKD.
There may be other mechanisms at play as well. Cyst fluid contains a factor that promotes cell growth and fluid production, and it has been identified as a molecule similar to forskolin, which can increase cAMP. It’s also possible that decreased signalling through a protein called Gi, which regulates AC activity, could lead to higher cAMP levels. Additionally, abnormal activation of a protein called GSK3β has been shown to contribute to elevated cAMP levels in the collecting ducts.
https://www.ncbi.nlm.nih.gov/books/NBK373395/
https://www.frontiersin.org/articles/10.3389/fphys.2021.693130/full
https://www.ncbi.nlm.nih.gov/books/NBK373395/
Crystals and PKD
The correlation between urinary crystals and ADPKD is examined in several studies, revealing several connections. Firstly, clinical kidney stone disease is observed in approximately 20% to 28% of ADPKD patients. Secondly, ADPKD is more prevalent in individuals with kidney stones. Thirdly, a significant proportion of ADPKD patients exhibit higher than normal levels of calcium oxalate (CaOx) in their urine, with nearly a fifth displaying elevated CaOx levels, around a quarter experiencing gout (a condition associated with uric acid crystals in the joints), and over 60% having elevated uric acid levels. All these factors are linked to the formation of oxalate and uric acid crystals. Uric acid crystals specifically contribute to accelerated cyst growth in ADPKD. It is worth noting that, similar to ADPKD, kidney stones tend to occur more frequently in males than females.
In addition to the findings above, scientific studies have also looked at the impact of crystal growth on the speed of cyst formation. Researchers have identified a previously overlooked mechanism called tubule dilation, which is crucial in eliminating microcrystals from the kidney.
Tubule dilation, which had been observed in previous research, is now recognised as a
protective mechanism against crystal-induced damage. It promotes the rapid passage of microcrystals through the renal tubules.
The renal tubules serve as the kidney’s filtration units and comprise various segments, including the proximal tubule at the beginning, the loop of Henle with ascending and descending limbs, and the distal tubule at the end, leading to the collecting ducts that drain the filtered urine into the collecting system.
When CaOx crystals are present in the kidney, the mTOR and Src/STAT3 signalling pathways become active. This activation leads to dilating the affected renal tubule along its entire length, including the collecting duct. Notably, these same pathways are active in ADPKD and contribute to cyst growth.
The mTOR pathway regulates the size and rate of proliferation in the tubular epithelium. It induces changes in cell shape through the actin cytoskeleton, resulting in cell flattening as the tubular diameter increases. It also causes cell cycle arrest in the G1 stage, indicative of hypertrophy or an increase in cell size rather than number. Upon deactivation, the normal cell cycle resumes.
Inhibition of the mTOR molecule prevents tubule dilation, leading to the formation of stones. This inhibition allows microcrystals to accumulate at the bottleneck where the proximal tubule transitions to the thin descending loop of Henle, which is the narrowest part of the tubule. Conversely, after approximately seven days of therapy targeting CaOx crystals, the tubule diameter returns to normal.
Supporting the hypothesis that CaOx crystals serve as the “third hit” triggering cyst formation and growth, the study found that chronic exposure to these crystals results in the deposition of CaOx crystals in male rats (but not females) with PKD, leading to increased disease severity. Another rat model also demonstrates similar effects with increased dietary phosphorus.
Furthermore, primary hyperoxaluria 1, a genetic disorder characterised by the accumulation of oxalate crystals in the kidney and eventual kidney failure, exhibits mTOR/STAT3 activation and dilated renal tubules. In ADPKD patients, the severity of the disease is inversely related to citrate levels in urine.

https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6763267/
https://www.futurity.org/polycystic-kidney-disease-cysts-2148362-2/
Above, I have gone through the major known biochemical processes that contribute to the formation of cysts in the PDK model. It is important to remember that PKD is a genetic disorder, so mutations in one of two genes, PKD1 or PKD2, account for most cases of ADPKD. The two disease loci segregate independently since they reside on separate chromosomes. The PKD1 gene is located on chromosome 16p13. 3, and the PKD2 gene is located on chromosome 4q21.
While genetic conditions are believed to be relatively unresponsive to any form of interventions, be it either pharmaceutical or a more natural approach, I believe differently. We are seeing how specific interventions like a ketogenic diet can profoundly impact slowing and even shrinking the growth of the cysts formed in the PKD model. And while most interventions are centred around mitigating the glycolysis pathway and cutting off glucose sources to starve off the fuel that contributes to the growth of the cysts, my scientific brain wonders what would happen if we had interventions that worked on all the pathways I covered above.
In the following article, I am going to cover just that. A PKD plan that we use is aimed at mitigating all the pathways I have covered above through not only dietary intervention but also the use of nutritional and herbal medicines.
Stay tuned.
Share This Article
More articles by
Fiona Chin N.D.
LIKE WHAT YOU’VE READ?
Sign up for free updates delivered to your inbox. Join our community and get tips on health, wellness, nutrition, and more.
More From Our Blog

The Oral Microbiome & Chronic Kidney Disease
The oral microbiome plays an essential role in the incidence and development of

Natural Therapies In The Treatment of Polycystic Kidney Disease
Regarding dietary interventions in treating and managing PKD, the science is solid. The
Bicarbonate Supplements? Is It The Best Way To Alkalize in Kidney Disease?
Throughout the ages, human diets have undergone a significant transformation, shifting from an

The Big Question… Can Kidney Disease Be Reversed?
Kidney disease can range from mild to severe, so the potential for reversal
SS-31 Peptide and Kidney Disease
Kidney disease is a global health concern. The kidneys, especially the proximal tubules,

The Role of Calcium in Kidney Disease
Calcium is the most abundant mineral in our body; ninety-nine per cent of